
The tale will one day be told?
About how the world came to a standstill as the year 2020 turned upside down. No one saw it coming.
The last time anything like this happened was in 1918. Then, the Spanish flu killed more than 2 million people.
The coronavirus disease 2019 (COVID-19) became a pandemic in 2020. Was history repeating itself?
The contagious respiratory disease was first identified in December 2019 in Wuhan. Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) was the relentless invisible ghost.
In desperate search for therapeutics and vaccines, scientists and researchers alike worked around the clock. The race to protect humankind was on.
This relentless invisible ghost had to be stopped!
In came biotechnology with the unique opportunity to speed up the search for new drugs. By now, we had more advanced scientific tools at our disposal than ever existed before. The secret weapon to fighting this common enemy was our immune system.
Scientific advances in molecular biology, genomics, bioinformatics and supercomputing became our ally. It was only a matter of time before the convergence of these disciplines won the battle.
We desperately needed a solution to overcome this pandemic.
Where did all this begin?
What started off as a zoonotic infection quickly established in the human population. Human-to-human infections became our Achilles? heel, and globalization, our undoing.
SARS-CoV-2, the enveloped RNA virus, is a second-generation daughter of the 2003 SARS virus. As is typical of RNA viruses, mutations generated SARS-CoV-2. It became 1000X more infective than the original SARS.
COVID-19 begins when the virus docks onto ACE2 receptors in the lungs. It establishes an initial respiratory infection that quickly becomes systemic. It overwhelms the immune system in some individuals, leading to various degrees of pathology. Three categories of patients have been described:
- Asymptomatic cases who account for more than 70% of all infected persons.
- About 20% of patients develop mild to moderate flu-like illness.
- Approximately 10% of infected patients develop severe outcomes. They experience lung injury and damage that causes pneumonia. These patients need hospitalized ventilation. Unfortunately >50% of them become critically ill leading to fatality.
What is the difference between a vaccine and an antiviral drug?
A vaccine is designed to train and educate your immune system to recognize SARS-CoV-2. A vaccine comprises parts of the virus (the antigen) that will interact with your immune system to trigger an antibody response. It typically will be administered as a prophylactic before infection. In case of a future infection, your body will be ready to defend itself.
Vaccine technologies have evolved over time but their applications remain the same.
Since SARS CoV-2 is an evolving virus, the ideal vaccine would be targeted to the stable conserved regions of the structural proteins. The aim is to elicit the strongest immune response. Luckily, the receptor-binding domain of this virus is conserved. Herein lies the key to implementing this strategy.
Antivirals, on the other hand, target virus-specific events. They are applied post-infection. They form the bulk of therapeutic approaches for critically ill patients.
At the point of writing this article, there were no antiviral treatments with confirmed activity against COVID-19. Clinical experiences from treating other illnesses with similar symptoms to COVID-19, formed the treatment baseline.
What is in the scientific horizon?
Stopping SARS-CoV-2 propagation in an infected person minimizes the risk of transmission. This became the argument for the selected therapeutic strategies.
The solution lies in understanding the science behind SARS-CoV-2 propagation. If we can understand the host?s reactions to SARS-CoV-2, then we can develop countermeasures. It all begins with understanding the dynamics of this virus.
What biotech therapeutic strategies are currently possible?
Therapeutic strategies have to be tailored to the disease severity.
1. Before a person is infected, two strategies can be applied:
- Vaccination (refer to previous description of a vaccine for details).
- Blocking the entry of the virus by obstructing access to the ACE2 receptor. The ACE2 receptor is the first port of entry of this virus. It is hijacked by SARS-CoV-2 to start an infection in the lungs. By obstructing this entry portal to lung tissue, we can prevent the entire cascade of the virus infection cycle.
Through the power of proteomics, the 3D structure of ACE2 is now fully understood. Decoys compatible to the receptor's active sites can be developed as prophylactics.
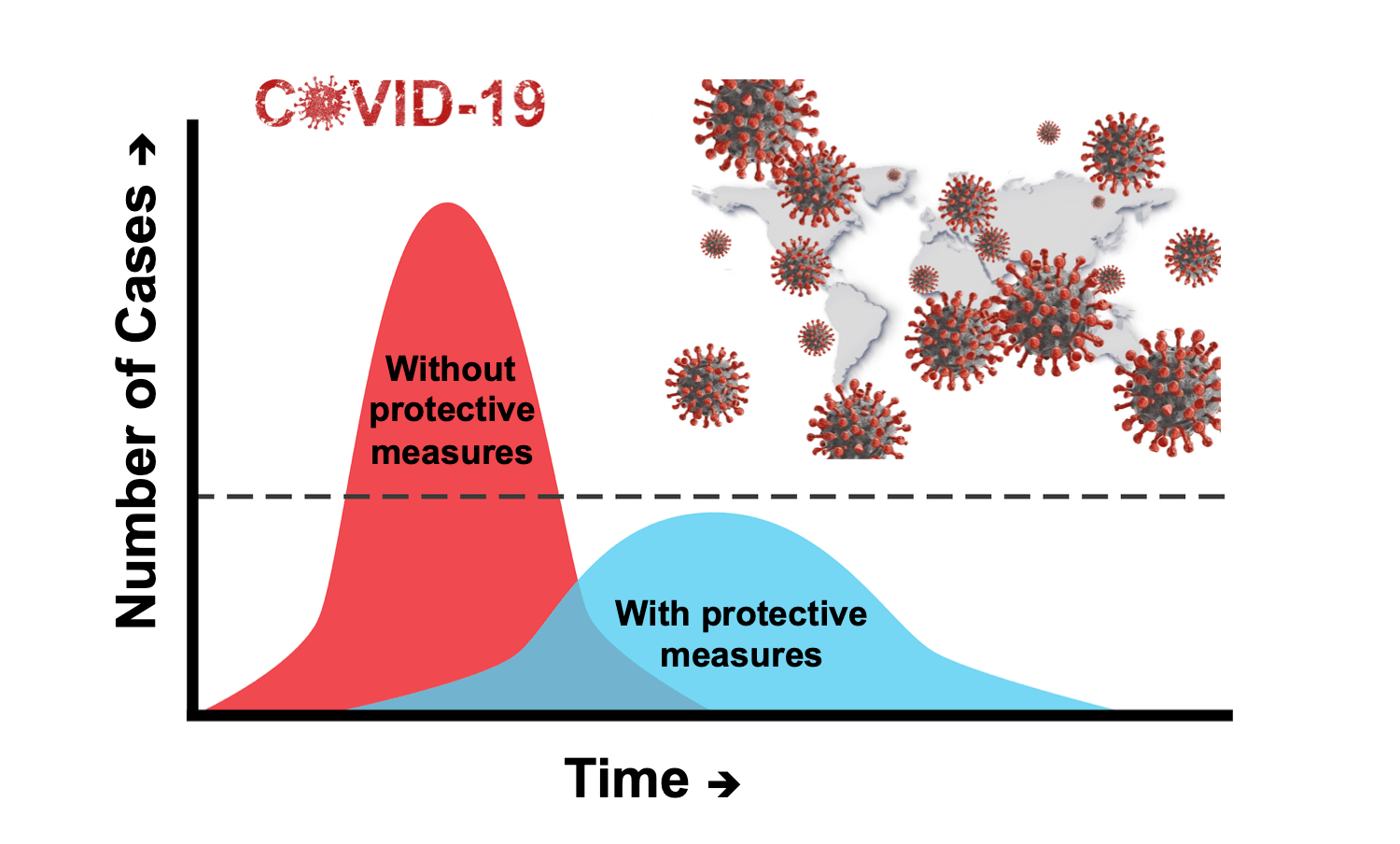
2. Asymptomatic cases can be managed by containment. Self-isolation is designed to limit and avoid further spread on the virus in the population.
3. The progression of COVID-19 from a mild infection to a critical illness depends on the integrity of the patient?s immune system. Pre-existing morbidities compromise the immune system.
The treatments for patients with mild to moderate symptoms should strengthen their immunity.
- First, blocking the entry of the virus by obstructing access to the ACE2 receptor. This is designed to slow down secondary infections of healthy cells in the body.
- Second, immunomodulatory drugs to prevent the fusion and packaging of the virus particles at the end of the replication cycle. The idea here is to slow the progression to the critical stage. These drugs should allow the immune system to fight the virus to full recovery.
- Third, blocking the virus replication machinery. Viruses survive by hijacking the replication machinery of the host cell. Antiviral drugs can trick the virus to misread its sequences and create crippling damage to its own genetic code.
- Finally, killing the infected cells that are actively replicating the virus in the body. The patient can be assisted to activate their natural killer cells. These are specialized lymphocytes of the innate immune system. They identify and destroy cells infected by the virus. The goal here is to destroy the infected cells by activating natural killer cells. The target is the factory itself. Activation of natural killer cells also induces some memory to the immune system.
4. When patients go into the red state, disaster hits. The virus has progressed so far that they develop full-blown SARS. Critical organs in the body are inflamed and fibrosis in the lungs causes scarring which prevents oxygen exchange.
In severely ill and critical patients, the viral load is huge. The immune system is overactivated and the response causes the body to turn on itself. The patients experience a cytokine storm in their lungs. The virus has spread so far and replicated in the body to an extent where they cannot breath without mechanical help.
When the patient?s immune system is fighting so hard it ends up being the cause of the damage caused.
The therapeutic strategy here is to reverse the disease progression. In this subset, calming the storm is the key to survival. While immunosuppression is beneficial in later phases of COVID-19, it can delay virus clearance when applied too early. A few candidate drugs rely on this premise.
In conclusion
These opportunities give us hope and some level of comfort. The world working together can stop a pandemic in its tracks.
Discover how a Technical Life Science Copywriter can help you communicate innovations effectively for greater public acceptance. Also, get to know blind spots in your website that affect how your content performs. Schedule your FREE diagnostic site content review to find out.